Neck of Femur (NOF) Fractures
Quick Links...
Related Topics...
More topics coming soon!
Background
Occurs most commonly in the elderly population following low energy falls. (1)
Can occur in younger patients if high energy mechanism. (1)
More common in women than men. (1)
Despite its’ seemingly low energy mechanism, these fractures carry a high risk of significant morbidity and mortality for patients. (1)
High Yield Anatomy to Know…
- Parts of femur
- Hip joint
- Blood supply of head of femur (medial femoral circumflex artery)
- Piriformis
- Superior gluteal artery
- Sciatic Nerve
- Lateral femoral cutaneous nerve
- See (2)
Presentation
History of fall – patients will also often have history of other comorbidities.
Pain in groin.
Inability to weight bear.
Pain with minimal active or passive hip movements.
Affected leg may be externally rotated, abducted, with shortening.
Management
ABCDE – Check neurovascular status of the limb!
Analgesia as per pain requirements. (3)
- Paracetamol
- Opioids if paracetamol not sufficient
- Can consider never blocks if paracetamol and opioids do not provide sufficient preoperative pain relief, or to limit opioid dosage.
- Fascia iliaca blocks can be for analgesia and are relatively safe to administer.
- Femoral nerve blocks can be used to provide additional blockade during surgery, however, carry greater risk of vessel damage.
- Non-steroidal anti-inflammatory drugs (NSAIDs) are not recommended. (3)
Further important considerations…
- Social Hx – thinking discharge planning
- Any anticoagulation regular medication?
- Any other medications need to stop/change prior to surgery?
- Any polytrauma?
- Long lie? – ?rhabdomyolysis, check CK
- Other bloods: FBC, U&E, coag, group&save
- Does cause of fall need exploring? – ECG
Imaging –
- XR Hip and pelvis:
- AP
- Lateral
- MRI if hip fracture is suspected despite negative X‑rays of the hip of an adequate standard. If MRI is not available within 24 hours or is contraindicated, consider CT. (3)
Types of NOF#
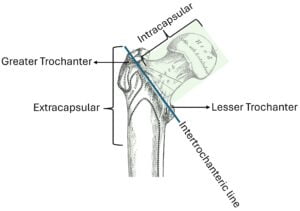
Broadly NOFs can be categorised relative to the joint capsule into intracapsular or extracapsular.
Simply…
- Intracapsular being proximal to the intertrochanteric line.
- Extracapsular being distal to the intertrochanteric line.
Intracapsular can be further specified…
- Sub-capital (base of the head)
- Transcervical (across the neck)
- Basi-cervical (base of the neck)
Extracapsular is further sub-divided into…
- inter-trochanteric – between the greater and lesser trochanter.
- sub-trochanteric – distal to the lesser trochanter.
Treatment Options
Non-operative
- May be considered in very few patients who are non-mobile with minimal pain and high risk for surgery.
Operative
- Surgery should be performed on the day of, or day after, admission (3).
- The type of surgery required depends on the 1) location of the fracture, 2) degree of displacement, and 3) the patient’s pre-injury status.
- The goal of all hip surgery is to aim to allow them to fully weight bear (without restriction) in the immediate postoperative period (3).
The need for surgical intervention is due to the retrograde nature of the blood supply (predominantly from the medial femoral circumflex artery), therefore, there is high risk of damage to the blood supply following an intracapsular fracture and subsequent avascular necrosis of the head of the femur.
Intracapsular
If the fracture is intracapsular the patient will likely require either a hemiarthroplasty or a total hip replacement (THR) (3).
If the fracture is incomplete, or not displaced, it may be fixed with cannulated hip screws (see Garden Classification).
A total hip replacement (THR) is preferred in patients who…
- Prior to injury were able to walk independently outside with no more than a stick AND
- Do not have a co-morbidity that makes them unsuitable for the procedure AND
- Are expected to be able to carry out activities of daily living independently beyond 2 years (3).
In summary…
Hemiarthroplasty = quicker less complicated surgery, but less post-op joint mobility.
THR = longer more complex surgery, but greater post-op joint mobility. Thus, reserved for more fit and able-bodied patients.
The Garden Classification is often used to further classify intracapsular fractures and guide management…
Garden Classification | Description |
I | Incomplete |
II | Complete, not displaced |
III | Complete, partially displaced |
IV | Complete, fully displaced |
There is a useful aide-memoir to help with the Garden Classification…
1, 2 … screw,
3, 4 … needs more.
i.e. if the fracture if a classification 1 or 2 (nondisplaced), it can be fixed with cannulated hip screws, if 3 or 4 (displaced) it will need either a hemiarthroplasty or total hip replacement.
Extracapsular
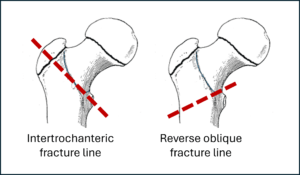
- Intertrochanteric # – can be managed with dynamic hip screw (DHS) and plating, unless there is evidence of a reverse oblique fracture (3).
- Reverse oblique # – this is a more unstable fracture, it should not be seen as a classic intertrochanteric fracture, this is treated with an intermedullary (IM) nail.
Picture this fracture as almost a mirror image of an intertrochanteric fracture, where the fracture line extends from the medial cortex out through the lateral cortex.
- Sub-trochanteric # – this is a more unstable fracture, so a IM nail is often used to manage these fractures (3).
Guidelines
Hip fracture: management. Clinical guideline [CG124] Published: 22 June 2011 Last updated: 06 January 2023 (3)
https://www.nice.org.uk/guidance/cg124
BOAST – The Care of the Older or Frail Orthopaedic Trauma Patient
https://www.boa.ac.uk/resource/boast-frailty.html
References
- Li L, Bennett-Brown K, Morgan C, Dattani R. Hip fractures. Br J Hosp Med Lond Engl 2005. 2020 Aug 2;81(8):1–10.
- Onyemaechi N, Anyanwu E, Obikili E, Ekezie J. Anatomical Basis for Surgical Approaches to the Hip. Ann Med Health Sci Res. 2014;4(4):487–94.
- Overview | Hip fracture: management | Guidance | NICE [Internet]. NICE; 2011 [cited 2024 Mar 5]. Available from: https://www.nice.org.uk/guidance/cg124
- Images adapted from: Gray H. Anatomy of the human body [Internet]. Philadelphia: Lea & Febiger; 1918 [cited 2024 Apr 15]. Available from: https://www.bartleby.com/lit-hub/bibliography/anatomy-of-the-human-body/