Galeazzi Fracture-Dislocation
Quick Links...
Related Topics...
Background
- Galeazzi Fracture-Dislocation consists of a fracture of the distal 1/3 of the radial shaft, with an associated distal radioulnar joint (DRUJ) dislocation.
- This presentation has a bimodal distribution, occurring in young males following high energy mechanism and older females following lower energy mechanism (1).
- Classification (1,2):
- They can be classified as per the direction of ulna subluxation:
- Volar
- Dorsal
- Can also be classified as per fracture location:
- <7.5cm distance from the midarticular surface of the distal radius (i.e. distal 1/3) – greater chance of significant DRUJ instability
- >7.5cm distance from the midarticular surface of the distal radius (i.e. middle 1/3) – smaller chance of significant DRUJ instability
- They can be classified as per the direction of ulna subluxation:
High Yield Anatomy to Know…
- Bones of forearm
- Carpal bones
- Median Nerve course
- Muscle compartments of the forearm
- Triangular fibrocartilage complex (TFCC)
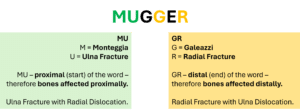
Galeazzi vs Monteggia
Many people may confuse these eponymous names with the respective similar fracture-dislocation presentation.
Therefore, the following aide memoir may be of use during this learning process…
Just remember the word ‘Mugger’ and that the aide memoir only refers to the fracture – so you just need to remember the other bone (not the fractured bone) is dislocated.
Presentation
- Most commonly a result of a fall onto an outstretched hand (FOOSH).
- Wrist pain, swelling, bruising, deformity.
- Movement limited by pain.
Management
- ABCDE
- Appropriate analgesia (3)
- oral paracetamol for mild pain
- oral paracetamol and codeine for moderate pain
- intravenous paracetamol supplemented with intravenous morphine titrated to effect for severe pain.
- Do not offer non-steroidal anti-inflammatory drugs (NSAIDs) to frail or older adults with fractures.
- Exclude compartment syndrome
- Assess median nerve sensation and motor (thenar weakness)
- Assess vascular status
- Skin condition?
- X-ray at least AP and lateral
- Social Hx – thinking discharge planning
- Any anticoagulation regular medication?
- Any other medications need to stop/change prior to surgery?
- Any polytrauma?
- Long lie? – ?rhabdomyolysis, check CK
- Other bloods: FBC, U&E, coag, group&save
- Does cause of fall need exploring? – ECG
- Bone health? – osteoporosis?
Imaging...

- X Ray: AP, Lateral, Oblique of Forearm, Elbow, Wrist
- Comment on…
- Radial fracture…
- Location
- Angulation
- Degree of Shortening
- Unla subluxation…
- Direction
- Radial fracture…
See ‘The Orthopaedic X Ray’ for more information on fracture description/presentation.
Treatment Options...
Due to the unstable nature of this fracture, in adults, all will require open reduction and internal fixation (ORIF) (1,4).
In children, conservative management with manipulation (closed reduction) and above-elbow casting can be considered. Surgical management (ORIF) may be required if adequate reduction cannot be achieved (1,4).
Guidelines
Fractures (non-complex): assessment and management
NICE guideline [NG38]Published: 17 February 2016
https://www.nice.org.uk/guidance/ng38/chapter/Recommendations
BOAST – Early Management of the Paediatric Forearm Fracture. 21 May 2021.
https://www.boa.ac.uk/resource/boast-early-management-of-the-paediatric-forearm-fracture.html
References
- Johnson NP, Smolensky A. Galeazzi Fractures. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 [cited 2024 Apr 22]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK470188/
- Rettig ME, Raskin KB. Galeazzi fracture-dislocation: a new treatment-oriented classification. J Hand Surg Am. 2001 Mar;26(2):228–35.
- Recommendations | Fractures (non-complex): assessment and management | Guidance | NICE [Internet]. NICE; 2016 [cited 2024 Apr 19]. Available from: https://www.nice.org.uk/guidance/ng38/chapter/Recommendations#management-in-the-emergency-department
- Atesok KI, Jupiter JB, Weiss APC. galeazzi Fracture. JAAOS – Journal of the American Academy of Orthopaedic Surgeons. 2011 Oct;19(10):623.