Prostate Cancer
Quick Links...
Related Topics...
Background
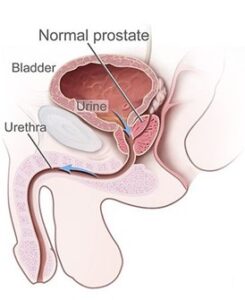
The prostate gland is part of the male reproductive system and is shaped like an inverted pyramid. Anatomically, it can be found sitting inferior to the neck of the bladder, surrounding the prostatic urethra (1).
Prostate cancer is the most common cancer found in men (2).
1 in 6-8 men will develop prostate cancer in their lifetime and approximately 50000 men are diagnosed each year (2, 3).
92% of all prostate cancers are adenocarcinomas (2).
Risk factors for developing prostate cancer include increasing age, being of an Afro-Caribbean ethnicity, and having a family history of prostate cancer (2).
Presentation
Prostate cancer is very often asymptomatic in many men, especially in the early stages.
Signs and symptoms can include:
- Lower Urinary tract symptoms: Bladder outflow or obstructive issue, including hesitancy when initiating urination, disruption to the flow of urine, nocturia, urgency and dribbling at the end of urination. An obstruction can lead to urinary retention.
- Blood: haematuria or haematospermia
- Pain: either in the testicles, perianal area, or back pain (secondary to spinal metastases)
Note that these signs and symptoms could be attributed to many conditions. These include: benign prostatic hyperplasia, prostatitis, urinary tract infection, and diabetes mellitus.
When considering what investigations to request, all these potential differential diagnosis should be in mind.
Diagnosis & Management
PR examination
- Findings: a hard, nodular, asymmetrical prostate.
Remember to explain this examination clearly to the patient before starting, gain consent and offer a chaperone!
You cannot exclude a diagnosis of prostate cancer with a digital rectal exam as it is only possible to examine one anatomical aspect of the prostate.
Investigations
- Prostate Specific Antigen (PSA)
- FBC and CRP for any signs of infection as infection in the urinary tract could skew the PSA result
- Urine dip – a UTI would skew the PSA result and explain urinary symptoms
- HbA1c – would explain an increase in urinary frequent and nocturia
- MRI (secondary care – see referral criteria)
- Prostate Biopsy (secondary care – see referral criteria)
The prostate gland produces PSA and is secreted into the prostatic fluid to liquify the semen. In men with an abnormal prostatic architecture, due to the presence of disease activity or a benign growth such as in benign prostatic hyperplasia, more PSA leaks into the blood than would be expected, hence producing an elevated PSA reading (2).
Therefore, an elevated PSA does not always mean that the patient has cancer, and equally a normal PSA result cannot guarantee that absence of prostate cancer. In fact only 15% of men who have an elevated PSA will go on to be diagnosed with prostate cancer (2).
PSA may be elevated for many reasons including benign prostatic hyperplasia, infection (e.g prostatitis, UTI), ejaculation (in the last 48hrs), procedures such as cystoscopy where there is instrumentation of the urinary tract, a digital rectal examination and even vigorous exercise (2).
Referral Criteria
According to NICE, patient should be referred on an urgent suspected cancer pathway if:
- the digital rectal examination reveals a prostate that feels malignant
- their PSA level is elevated for a person of that age
Those referred would be seen by a urologist for a Digital rectal examination (DRE), and if indicated will proceed to have an MRI followed by a biopsy of the prostatic tissue (2).
Gleason Grading System
The Gleason Scoring System is grading system for prostate cancer that is based on the examination of the biopsied prostatic tissue (4).
The score is out of ten.
- A score of ≤6 indicates a low grade tumour.
- A score of 7 indicates an intermediate grade tumour.
- A score of 8-10 indicates a high grade tumour.
The score considers two factors:
- the highest grade tumour (i.e the worst type of cancerous cell found in the biopsies)
- the most common type of cancerous cell present
Both factors’ scores would be out of five then added together to form the Gleason score.
So in a biopsy where the most common type of cell is a 2/5 and the highest grade is 5/5, the score would be 7.
Equally in a patient whose biopsies where the highest grade cells were a 5/5 and they were also the most common type of cell, that would be a Gleason score of 10 – the highest possible score.
Treatment
As per NICE guidelines the treatment options for prostate cancer are as follows (2):
Watchful waiting
- Aimed at patients who have localized prostate cancer who are not suitable for, or do not wish to receive, curative treatment.
- These are often older men or men with multiple co-morbidities who would not be suitable for more radical curative treatments. It is also suitable for men with slow growing tumours who are likely to die of other causes before the prostate cancer causes any significant morbidity.
- The focus is to control the disease rather than to cure it.
Active surveillance
- This is aimed at patients who are suitable for more radical treatment, but does not necessarily require it in the immediate.
- In an aim to avoid over-treating, active surveillance allows for the repeating of prostate biopsy at intervals and monitoring of the PSA for any signs that the tumour is progressing.
- If the prognostic risk category changes due to progression of the prostate cancer, this allows for intervention with either radiotherapy or surgery to be offered to the patient.
Radical/curative treatments
- Surgery – radical prostatectomy to remove the prostate gland and the lymph nodes to which it drains
- Radiotherapy
- External Beam Radiotherapy – this is a type of ionizing radiation aimed at the tumour from outside the body
- Brachytherapy – this involves inserting or implanting radioactive sources directly into the prostate. There are two types. High dose, which would be temporarily inserted into the prostate gland, or low-dose which would be permanently implanted.
Adjunct Therapies
- Chemotherapy
- Hormonal treatments: this involves depravation of, or blocking, Androgen hormones that would otherwise stimulate tumour growth.
- Androgen blocking involves using medications that bind to the hormone receptor, hence blocking the hormone from binding.
- Androgen deprivation involves using Luteinizing Hormone-releasing hormone agonist or antagonist to decrease the testosterone levels
Guidelines
NICE Prostate cancer Diagnosis and treatment:
https://www.nice.org.uk/guidance/ng131/evidence/full-guideline-pdf-6781033550
https://www.nice.org.uk/guidance/ng131/chapter/Recommendations
NICE CKS Prostate cancer:
https://cks.nice.org.uk/topics/prostate-cancer/
European Association of Urology – Guidelines on Prostate Cancer:
https://uroweb.org/guidelines/prostate-cancer/chapter/introduction
References
References
- Mahadevan GS, Arunachalam VK, Rajasekaran S, Kashyap R, Gunasekaran K, Thirumoorthi S. Anatomy of the Prostate Gland: Modalities and Techniques for Its Assessment. J Gastrointest Abdom Radiol [Internet]. 2024 Mar 26 [cited 2024 May 12]; Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/s-0044-1785197
- Prostate cancer | Health topics A to Z | CKS | NICE [Internet]. [cited 2024 May 7]. Available from: https://cks.nice.org.uk/topics/prostate-cancer/
- Cancer Research UK [Internet]. 2015 [cited 2024 May 7]. Prostate cancer statistics. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer
- Uroweb – European Association of Urology [Internet]. [cited 2024 May 11]. EAU Guidelines on Prostate Cancer – CLASSIFICATION AND STAGING SYSTEMS – Uroweb. Available from: https://uroweb.org/guidelines/prostate-cancer/chapter/classification-and-staging-systems